Once viewed as a measure of last resort, surgical interventions today offer a path to restoration and enhanced well-being. Yet, amid this progress, a silent adversary lurks—deep vein thrombosis (DVT). As we navigate the post-surgery journey, it’s high time we spotlight the crucial role of movement in warding off this potentially life-threatening complication. Let’s dive into the lifesaving connection between post-surgery activity and DVT prevention, unraveling strategies to keep this hidden danger at bay.
The Sneaky Foe: Understanding DVT
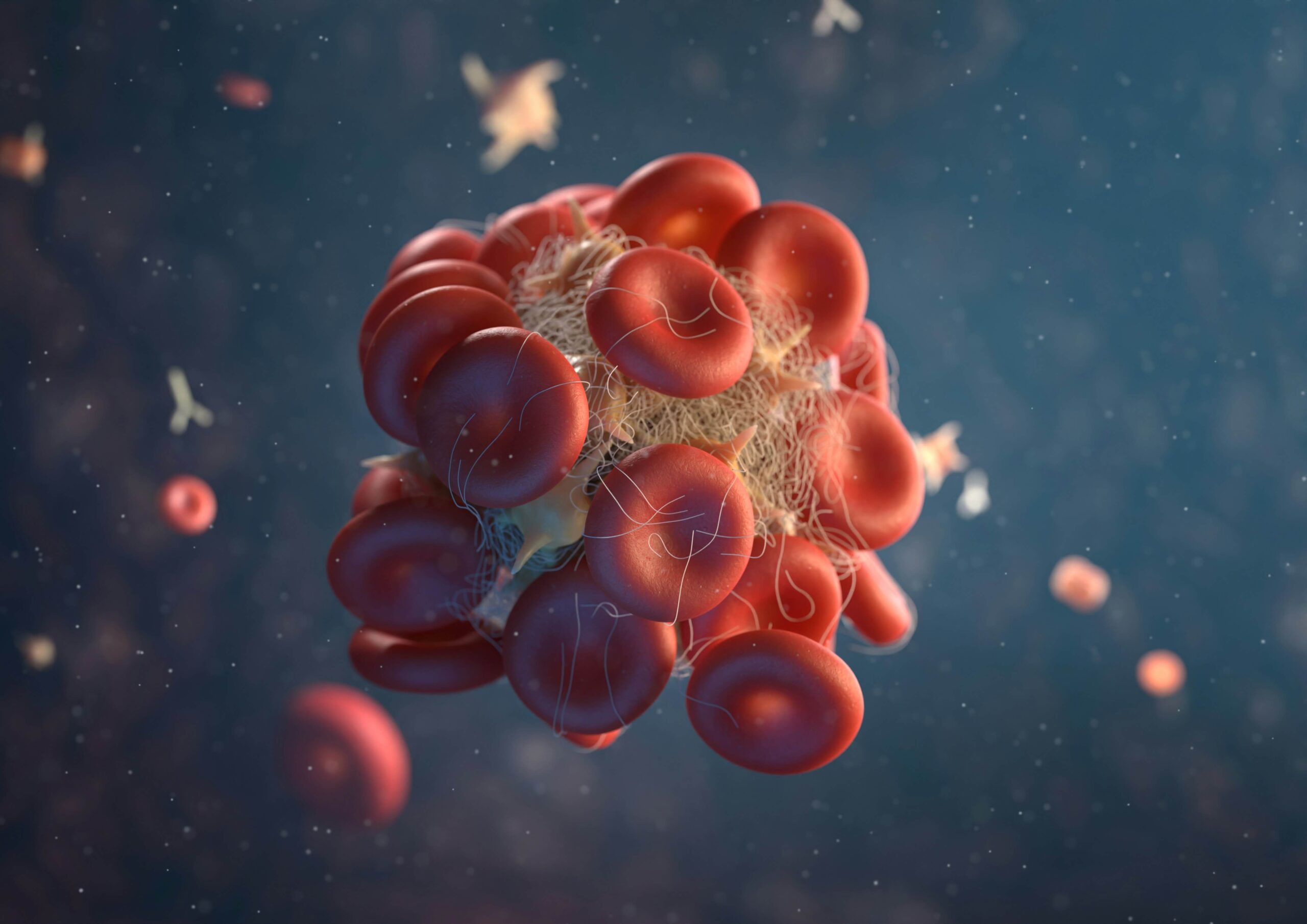
Imagine the bloodstream as bustling highways within our body. Picture DVTs as unexpected roadblocks disrupting this flow, primarily in the veins of the legs. These clots can embark on a perilous journey, potentially lodging in the lungs as a pulmonary embolism (PE)—a scenario we’re all keen to avoid. After surgery, when our bodies crave stillness, the risk of these dangerous clots forms silently. Why? Because immobility invites stasis, blood flow slows, and the conditions become ripe for clotting.
Symptoms of a DVT:
Deep vein thrombosis occurs without symptoms about 50 percent of the time. When symptoms do occur, they may include:
- Swelling in one or both legs
- Pain
- Warm skin or hot to touch
- Discoloration (bluish or reddish) of the skin
Mobilizing Against DVT: Science Takes the Stand
The evidence is compelling: movement is a potent foil to DVT’s plans. Studies across various medical specialties highlight a clear trend—surgical recovery, complemented by thoughtfully prescribed movement, significantly diminishes DVT risk. From gentle walks to tailored physiotherapy, the goal is clear—keep the blood moving.
A Prescription for Movement: Navigating Post-Surgery Recovery
Gone are the days when post-operative advice was to remain as still as possible. Today, the clarion call is for calculated movement. The sweet spot is between necessary rest and beneficial activity. Encouraging patients to take those first steps, to flex and extend gently, not only aids overall recovery but also turns the tide against DVT.

Charting the Path: From Hospital to Home
The journey doesn’t end upon discharge. Transitioning from the vigilant care of the hospital to the autonomy of home recovery, the emphasis on movement remains paramount. Here, the challenge shifts to adapting one’s living space to reduce fall risks and continue mobilizing safely. Assistive devices aren’t just tools but lifelines, enabling patients to navigate their homes and recover confidently.
Embracing Technology: A Modern Ally
In our digital age, wearable devices become unsung heroes, offering real-time insights into patient activity levels. When woven into care plans, this data can guide adjustments, ensuring that each patient’s road to recovery is as informed as it is individualized.
The Core of Recovery: Patient Empowerment
The journey back to wellness is a collaborative one. By arming patients with knowledge and supporting them through personalized exercise programs, we can foster an environment where post-surgery recovery is proactive, not just reactive. It’s about transforming patients into active participants in their journey back to health.
The Final Stride: A Collective Movement
Prioritize movement with a unified goal—to safeguard patients from the specter of DVT. It’s a call to action for healthcare professionals, patients, and caregivers to champion a culture where recovery is active, vigilant, and, most importantly, safe.

Conclusion: The Leap Beyond Surgery
The narrative of surgical recovery is evolving. It is no longer about surviving the operation but thriving in the aftermath. As we continue to push the boundaries of what’s possible in healthcare, let us pay attention to the basics. In its simplicity, movement holds the power to transform post-surgery recovery, making the journey back to health one to embrace. Together, let’s take this step forward, turning the tide against DVT and stepping into a future where surgery’s promise is fully realized, unmarred by preventable complications.